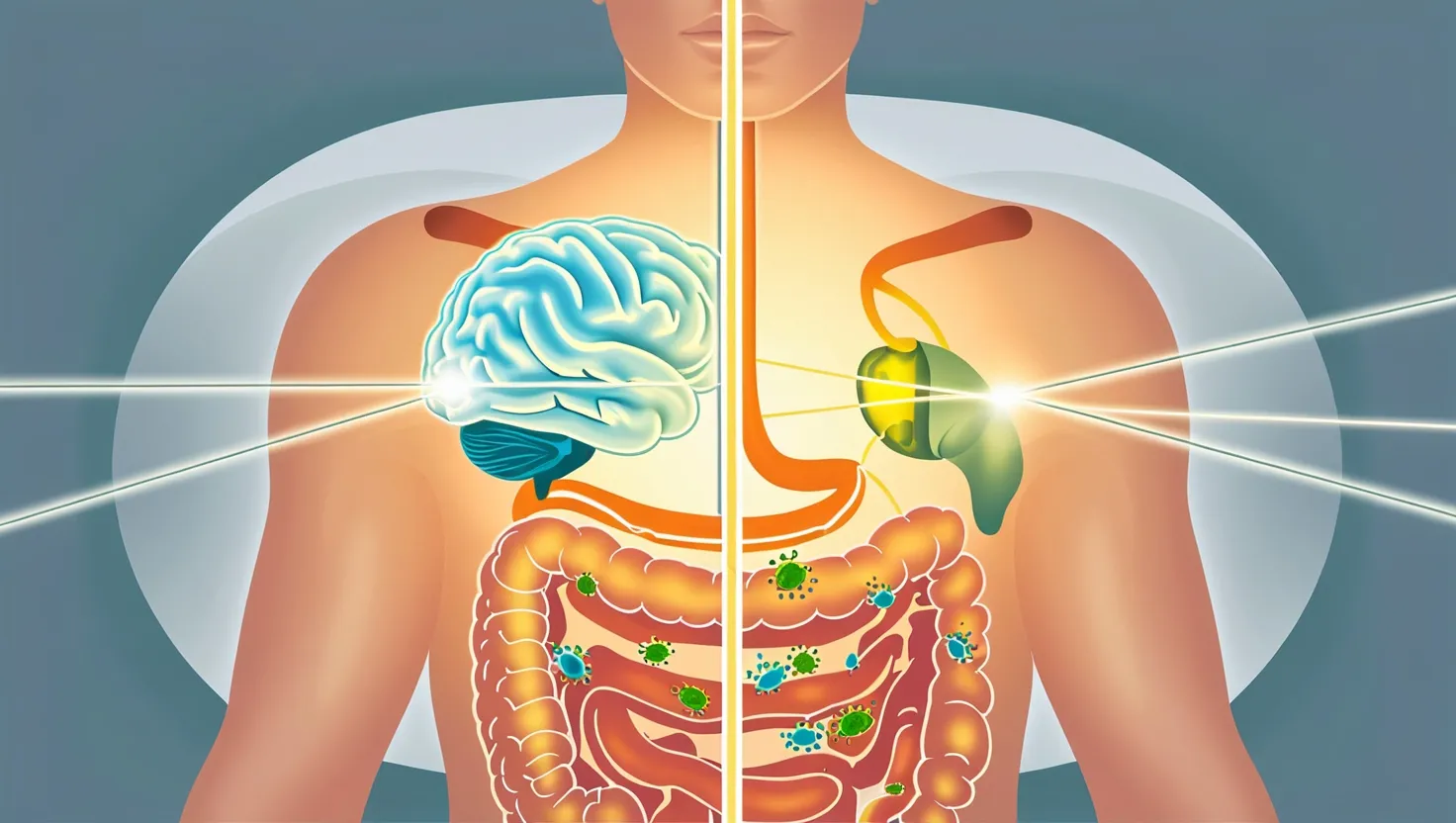
Let me start with a question: Have you ever had a “gut feeling” about something? Most of us have. But did you ever wonder why that phrase even exists? I want to take you on a simple journey into the world inside your own body—the mysterious conversation between your gut and your brain. This isn’t just about what happens when your stomach grumbles before lunch. I’m talking about a two-way communication system, a sort of “chat line” between your intestines and your thoughts.
This chat line is called the gut-brain axis. I know that sounds like a technical term, but you can think of it like a phone line, cables, and radio signals all running between your brain and your gut every single day. Here’s the fun part: scientists are discovering just how much our bellies and brains influence each other in ways we never guessed. We all know food gives us energy, and sometimes food can be comforting. But that’s only the start.
Let’s begin with those trillions of microbes living quietly in your intestines. Yes, you and I have an invisible population inside us, and without them, our health would be a lot worse. Some researchers even call our gut a “second brain” because it has its own little nervous system—with about 100 million neurons. I find it wild that’s more than the spinal cord. Imagine, a cluster of brain-like cells managing food, mood, and who knows what else.
Here’s something you may not know: those microbes actually make chemicals called neurotransmitters, the same kind that your brain uses to send messages. For example, most people hear about serotonin—sometimes called the “happy chemical.” But did you know that around 90% of your body’s serotonin is made in your gut, not your brain? Seems odd, right? And yet, this serotonin can start in the gut and send signals that change your feelings and reactions.
“Trust yourself. You know more than you think you do.” —Benjamin Spock
Why should serotonin, made in your stomach, affect whether you feel sad or anxious? This is still a mystery, but studies show that when the gut’s balance is disturbed—say, by antibiotics, illness, or stress—people can become more anxious or even depressed. That means part of our mental health may depend as much on having the right bacteria as it does on positive thinking or therapy.
Now, let me ask you this: Have you ever noticed your appetite change when you’re stressed? Maybe your stomach knots up before a big test or job interview. The nervous stomach is not just all in your head. Your brain sends signals to your gut and vice versa. If the brain is anxious, the gut reacts. But it’s a two-way street. Sometimes trouble in the gut—the wrong mix of microbes, inflammation, or irritation—can trigger negative emotions or even change how you make decisions.
Another fascinating thing is how quickly diet can shift the balance. There’s mounting evidence that what you eat today can affect your mood tomorrow. Eat a lot of processed food and the “good” bacteria might decrease, giving the “bad” microbes more room. That can lead to inflammation, which in turn may mess with your brain chemistry. Does this mean pizza causes sadness? Not exactly, but it does mean that nutrition has a much closer link to our emotions, memory, and even how we cope with stress than most people guess.
But here comes an even bigger puzzle: researchers have noticed that some diseases, like Parkinson’s and some forms of long-term cognitive fog, may start—not in the brain—but in the gut. That idea flips everything we thought about disease upside down. Parkinson’s, for example, shows signs in the intestines long before the tremors start. Does this mean we can spot or influence brain conditions by caring for our digestion? Possibly, but nobody is sure why.
Here’s a quote to consider:
“All disease begins in the gut.” —Hippocrates
Now, that’s a bold claim, and we shouldn’t take it too literally. But think about this: the gut isn’t just a simple food tube. It contains immune cells, bacteria, and its own nervous system. Diseases like irritable bowel syndrome often come with anxiety or depression, for reasons we still don’t fully understand. Scientists are investigating if unhealthy guts might actually cause some mental health problems or if it’s the other way around.
So, do changes in our mood lead to stomach trouble—or does stomach trouble lead to changes in our mood? The answer isn’t clear. That’s one of the biggest mysteries in this field.
What about quick fix diets? Plenty of companies now claim you can “fix your brain” by popping probiotics or eating special foods. Some evidence supports the idea that certain diets can help with depression or mental focus. But why do only some people benefit while others don’t feel a thing? The real answer probably involves the unique mix of bugs everyone has. No two people have the exact same gut community, so there’s no one-size-fits-all solution.
Did you know that nerves inside your gut, called the vagus nerve, run straight to your brainstem? This nerve acts like a busy phone line—signals travel along it in both directions, controlling things like heartbeat, breathing, and digestion. Stimulating the vagus nerve in certain ways can even help with depression in people where nothing else seems to work. It’s pretty wild to think a nerve connecting your stomach could shift your mood.
Here’s something else many people miss: childhood experiences—good or bad—can set the stage for how these gut-brain signals work as you grow up. Kids exposed to high stress or poor diets may end up with more sensitive guts and more “nervous stomachs.” It’s another reason why looking after our gut health is more than just about avoiding bloating—it might also be tied to our long-term mental well-being.
“Every man can, if he so desires, become the sculptor of his own brain.” —Santiago Ramón y Cajal
If this all sounds confusing, you’re not alone. Even the smartest scientists are still asking: Which comes first, the gut trouble or the brain trouble? Can we heal the brain by fixing the gut? Or are some problems too complex for us to patch up with probiotics and fiber?
Let me toss out a question for you: If scientists could create a simple pill or food to support the best gut-brain connection, would you take it? Or would you rather focus on more traditional ways of improving your mood and mind?
At this point, what we know for sure is pretty simple. Looking after your gut is good for you—eating more fiber, less junk, and not stressing too much about every meal is a smart place to start. The gut-brain connection is real and powerful, but still partly a black box. Sometimes, answers create more questions.
Here’s a closing thought for you: science now agrees that taking care of your mind and your belly are connected in unexpected ways. Every time you eat, your food becomes part of a silent conversation. By tuning in to that chat and treating your gut kindly, you might be helping both your stomach and your mood—even if we don’t know all the reasons why just yet.
“To know thyself is the beginning of wisdom.” —Socrates
So next time you get a gut feeling, maybe listen a bit closer. The answers to many problems, both big and small, may start from the inside out.